Eligibility and Enrollment
On this page:
Eligibility
Generally, a Medicare beneficiary is eligible to enroll in our Medicare Advantage plans if the following two conditions are satisfied:
- He or she is entitled to Medicare Part A and is enrolled in Medicare Part B as of the effective date of enrollment in one of our plans.
- He or she lives in the service area covered by one of our plans.
There are some exceptions to the general rule, and some other eligibility rules. Please contact Member Services for additional information.
At each office visit your office staff should:
- Ask for the member’s ID card.
- Copy both sides of the ID card and keep the copy with the patient’s file.
- Determine if the member is covered by another health plan to record information for coordination of benefits purposes.
- Refer to the member’s ID card for the telephone number to verify eligibility, deductible, coinsurance, copayments and other benefit information.
To view a member’s specific plan benefits, use the Plan number located on the ID card to find the Evidence of Coverage on our website.
Participating providers must admit patients to a participating facility unless an emergency situation exists that precludes safe access to a participating facility or if the admission is approved for a non-participating facility.
The member will receive in-network benefits only when services are performed at a participating MercyOne Health Plan provider.
Enrollment
There are limits to when and how often Medicare beneficiaries can change the way they receive their Medicare benefits:
- Between Oct. 15 and Dec. 7 each year, anyone can make any type of change, including adding or dropping Medicare prescription drug coverage.
- From Jan. 1 through March 31, anyone enrolled in a Medicare Advantage Plan (except those with an MSA plan) has an opportunity to change plans or return to Original Medicare. Anyone who disenrolls from a Medicare Advantage plan during this time can join a stand-alone Medicare Prescription Drug Plan during the same period.
Generally, you may not make changes at other times unless you meet certain special exceptions; such as if you move out of the plan’s service area, want to join a plan in your area with a 5-Star Rating or qualify for extra help with your prescription drug costs.
In general, Medicare beneficiaries are only able to change the way they receive Medicare benefits two times a year (as noted above).
There are special exceptions, for example: if beneficiaries move out of a plan’s service area, are institutionalized or have ‘Medicaid’ benefits.
The Member's Primary Care Provider (PCP)
Each member who enrolls in one of our HMO products is required to choose his or her own primary care provider (PCP) from a list of network providers. Each PPO member must choose his or her own PCP from a list of our network providers or an out-of-network provider.
Members have the option to change their PCP at any time upon request. Changes in PCPs are effective on the first day of the month after the request is processed by MercyOne Health Plan. MercyOne Health Plan will monitor the frequency and reasons members change PCPs. When MercyOne Health Plan determines that frequent changing of a PCP interferes with a PCP’s ability to effectively manage a member’s care, MercyOne Health Plan may limit the ability of a member to change his or her PCP.
To request a PCP change, members must call Member Services at toll-free 1-800-240-3851 (TTY: 711), or submit a written request to:
MercyOne Health Plan
Enrollment Department
Attention: PCP Change Request
3100 Easton Square Place
Suite 300 – Health Plan
Columbus, Ohio 43219
You may request a listing of members assigned to you by contacting provider services.
Membership Identification Card
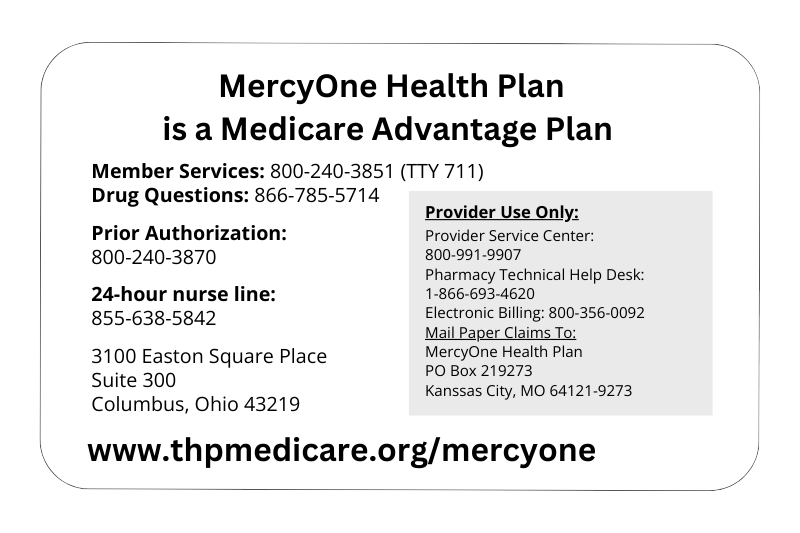
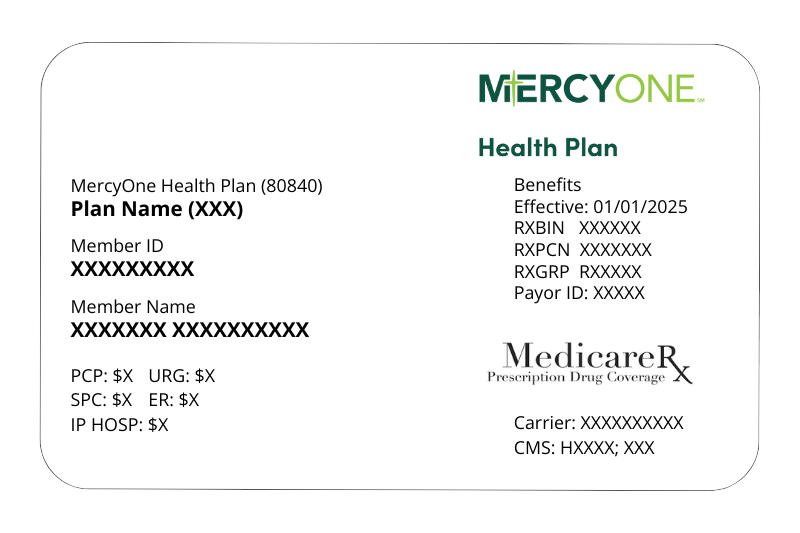
MercyOne Health Plan issues an identification (ID) Card to each member. Members are required to present their ID cards for medical, hospital, and other covered services. The member ID card will identify members to you and your staff and provides quick access to pertinent information such as applicable copays, contact numbers to coordinate medical care, hospitalization or other covered services, as well as claims submission information. Our members are instructed to put their Medicare cards away for safekeeping and present only their member ID cards at the time of service.
Be sure to check the member’s ID card at each visit, especially the first visit of each year when the information is most likely to change.
For reference purposes, a sample of our member identification card is included below.
2025 Member ID Card – Front
2025 Member ID Card – Back